
Introduction
Vitamin D plays a critical role in skeletal development and calcium homeostasis during childhood. Deficiency remains prevalent globally and is associated with rickets, impaired bone mineralization, and potential extra-skeletal health effects. This article summarizes the clinical impact, high-risk populations, screening considerations, and evidence-based management strategies for vitamin D deficiency in children.
Clinical Impact of Vitamin D Deficiency
Vitamin D deficiency significantly reduces intestinal calcium absorption, often to as low as 10–15%, leading to hypocalcaemia, secondary hyperparathyroidism, and defective bone mineralization. Clinically, affected children may present with bone deformities, bone pain, delayed growth, and, in severe cases, hypocalcaemic seizures.
Beyond skeletal outcomes, observational data suggest that adequate vitamin D status may be associated with a lower risk of certain autoimmune conditions, such as type 1 diabetes, and possibly some malignancies. Evidence for neuropsychiatric effects remains suggestive rather than conclusive.
Diagnostic Thresholds
Serum 25-hydroxyvitamin D [25(OH)D] is the recommended biomarker for assessing vitamin D status:
-
Deficiency: < 37.5 nmol/L (15 ng/mL)
-
Insufficiency: 37.5–50 nmol/L (15–20 ng/mL)
-
Sufficiency: ≥ 50 nmol/L (≥ 20 ng/mL)
High-Risk Groups
Certain pediatric populations are at increased risk of vitamin D deficiency, including:
-
Exclusively breastfed infants
-
Children with darker skin pigmentation
-
Adolescents, particularly during periods of rapid growth
-
Individuals with malabsorption disorders
Screening Recommendations
Routine population-wide screening is not universally recommended. Measurement of serum 25(OH)D should be considered in symptomatic children or those belonging to high-risk groups.
Treatment Strategies
Treatment approaches depend on severity and adherence considerations:
-
Daily therapy: Vitamin D 1,000–5,000 IU/day for 2–3 months, followed by maintenance dosing (approximately 400 IU/day)
-
Stoss therapy (for poor adherence): A single high oral dose of vitamin D (100,000–600,000 IU) administered over 1–5 days, followed by maintenance therapy
-
Adjunctive calcium supplementation is recommended when dietary intake is inadequate
Therapeutic Monitoring
Monitoring is essential to ensure efficacy and safety:
-
At 1 month: serum calcium, phosphorus, and alkaline phosphatase (ALP)
-
At 3 months: serum 25(OH)D, parathyroid hormone (PTH), calcium, phosphorus, and ALP
Radiographic evidence of healing may further confirm treatment response.
Reference: Misra et al., Pediatrics, 2008;122:398.
 The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc.
The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc. 50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others.
50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others. Single-dose Chemiluminescense Immunoassay Platform
Single-dose Chemiluminescense Immunoassay Platform Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously.
Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously. Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals.
Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals. Ready-to-use lyophilized RT-PCR Reagent;
Ready-to-use lyophilized RT-PCR Reagent; Wondfo PA-3600 IHC Staining System
Wondfo PA-3600 IHC Staining System The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds.
The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds. This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.
This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.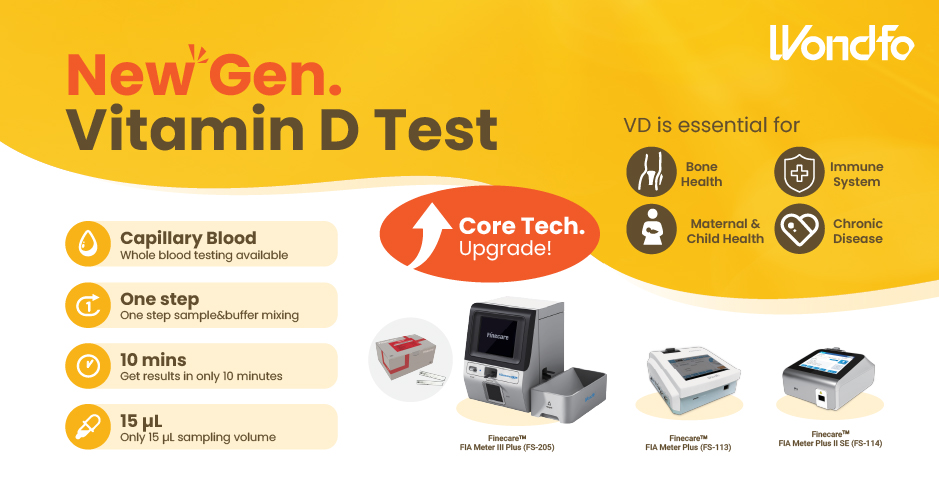 Finecare™ Vitamin D, from complexity to simplicity
Finecare™ Vitamin D, from complexity to simplicity Building A World Free from Antibitoic Overuse
Building A World Free from Antibitoic Overuse Advanced rapid diagnostic test with WHO prequalification for infectious disease
Advanced rapid diagnostic test with WHO prequalification for infectious disease The Future Intelligent Medical Assistant to Healthcare
The Future Intelligent Medical Assistant to Healthcare Fight against the pandemic through continuous innovation
Fight against the pandemic through continuous innovation




































