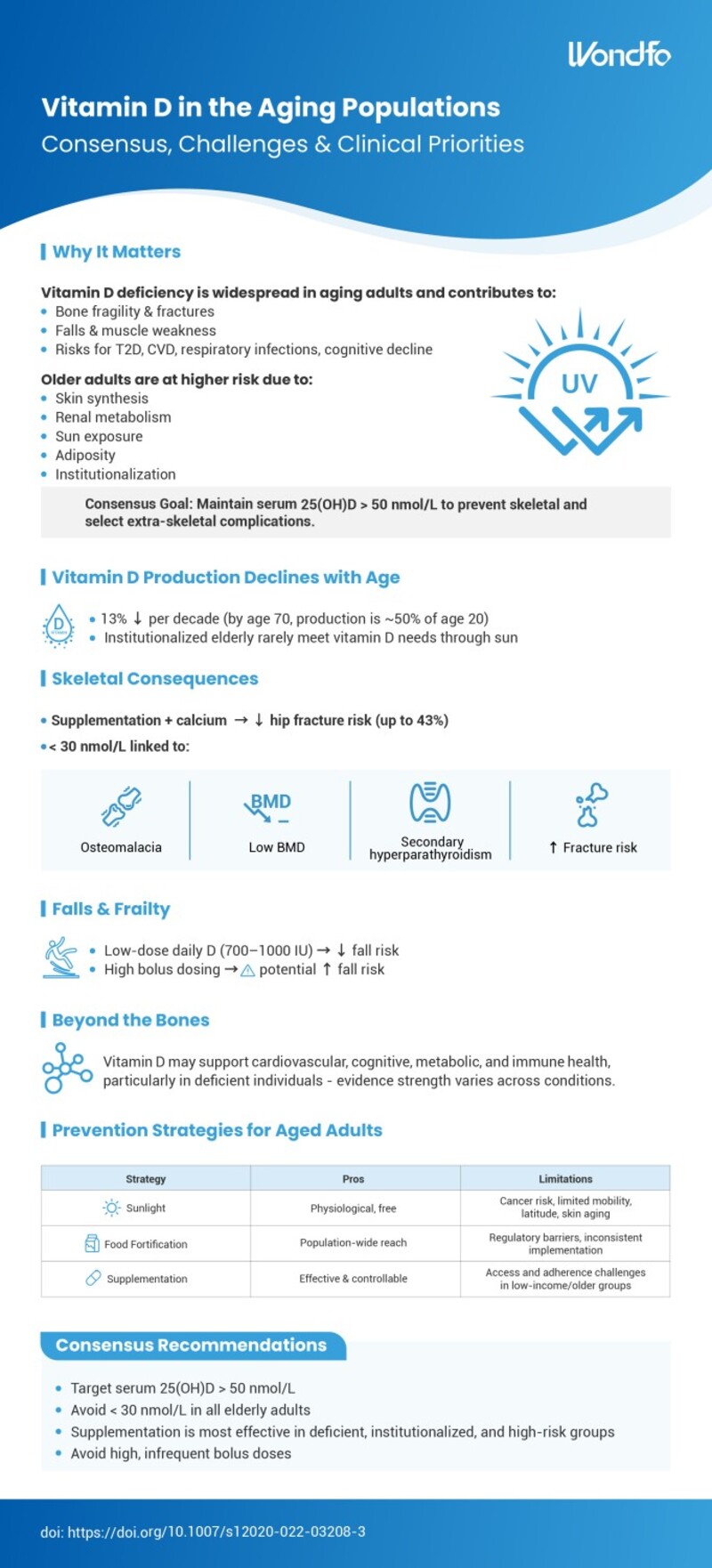
Vitamin D deficiency is highly prevalent among aging populations and represents a significant public health concern. In older adults, insufficient vitamin D status contributes to skeletal complications and may influence a range of extra-skeletal health outcomes, underscoring the need for targeted prevention and management strategies.
Why Vitamin D Matters in Older Adults
Vitamin D deficiency in older adults is associated with:
-
Bone fragility and increased fracture risk
-
Falls and muscle weakness
-
Elevated risk of type 2 diabetes, cardiovascular disease, respiratory infections, and cognitive decline
Aging populations are at higher risk due to reduced skin synthesis, altered renal metabolism, limited sun exposure, increased adiposity, and higher rates of institutionalization.
Consensus guidelines recommend maintaining serum 25-hydroxyvitamin D [25(OH)D] levels above 50 nmol/L to prevent skeletal and selected extra-skeletal complications.
Age-Related Decline in Vitamin D Production
Vitamin D production declines by approximately 13% per decade, with endogenous synthesis by age 70 reduced to roughly half of that at age 20. Institutionalized older adults rarely meet vitamin D requirements through sun exposure alone.
Skeletal Consequences
Vitamin D supplementation combined with calcium has been shown to reduce hip fracture risk by up to 43%. Severe deficiency (25[OH]D < 30 nmol/L) is associated with osteomalacia, low bone mineral density, secondary hyperparathyroidism, and increased fracture risk.
Falls, Frailty, and Dosing Considerations
Daily low-dose vitamin D supplementation (700–1,000 IU) is associated with reduced fall risk, whereas high intermittent bolus dosing may increase fall risk and should be avoided.
Beyond Skeletal Health
Vitamin D may support cardiovascular, metabolic, cognitive, and immune health, particularly in deficient individuals, although the strength of evidence varies across conditions.
Prevention Strategies in Older Adults
Preventive approaches include:
-
Sunlight exposure: Physiological but limited by cancer risk, mobility, latitude, and skin aging
-
Food fortification: Broad population reach but subject to regulatory and implementation challenges
-
Supplementation: Effective and controllable, though access and adherence remain concerns in low-income and elderly populations
Consensus Recommendations
-
Target serum 25(OH)D levels above 50 nmol/L
-
Avoid levels below 30 nmol/L in older adults
-
Prioritize supplementation for deficient, institutionalized, and high-risk groups
-
Avoid high, infrequent bolus dosing regimens
Reference:
doi: 10.1007/s12020-022-03208-3
 The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc.
The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc. 50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others.
50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others. Single-dose Chemiluminescense Immunoassay Platform
Single-dose Chemiluminescense Immunoassay Platform Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously.
Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously. Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals.
Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals. Ready-to-use lyophilized RT-PCR Reagent;
Ready-to-use lyophilized RT-PCR Reagent; Wondfo PA-3600 IHC Staining System
Wondfo PA-3600 IHC Staining System The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds.
The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds. This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.
This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.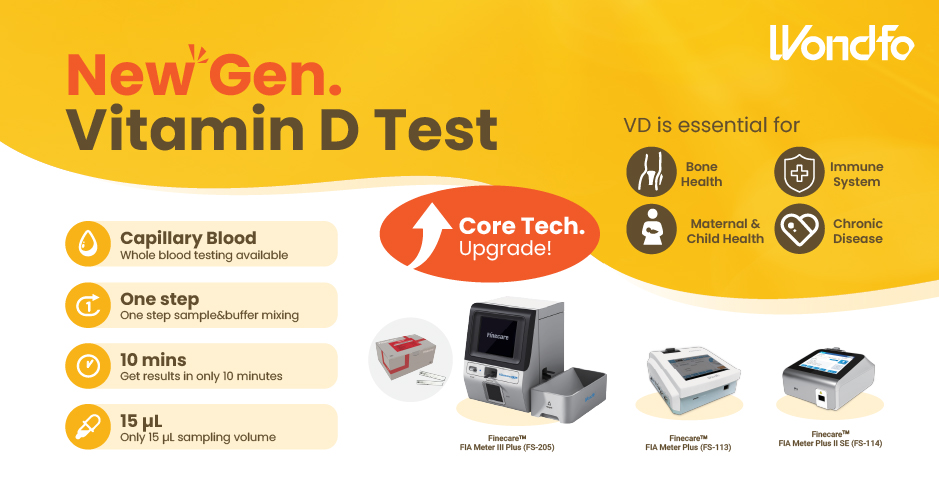 Finecare™ Vitamin D, from complexity to simplicity
Finecare™ Vitamin D, from complexity to simplicity Building A World Free from Antibitoic Overuse
Building A World Free from Antibitoic Overuse Advanced rapid diagnostic test with WHO prequalification for infectious disease
Advanced rapid diagnostic test with WHO prequalification for infectious disease The Future Intelligent Medical Assistant to Healthcare
The Future Intelligent Medical Assistant to Healthcare Fight against the pandemic through continuous innovation
Fight against the pandemic through continuous innovation