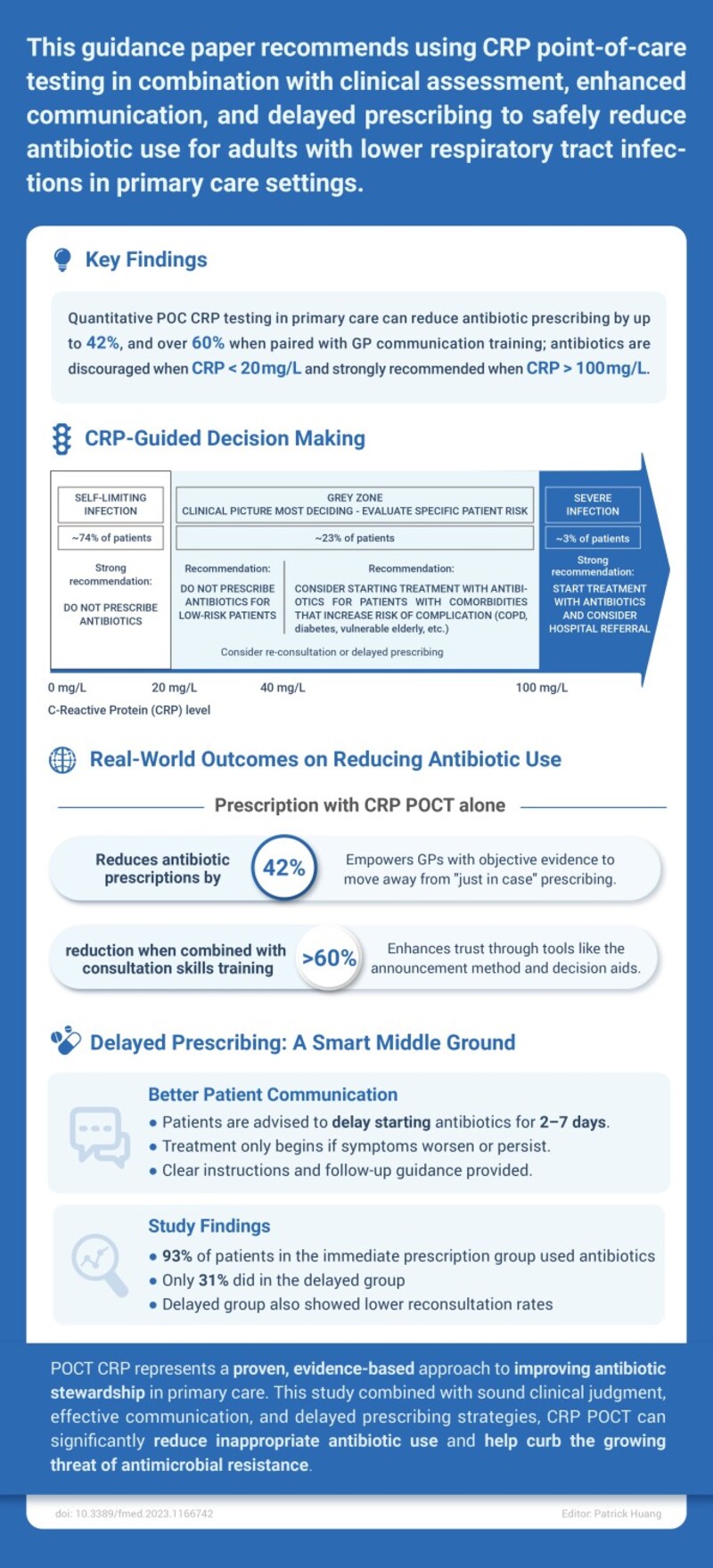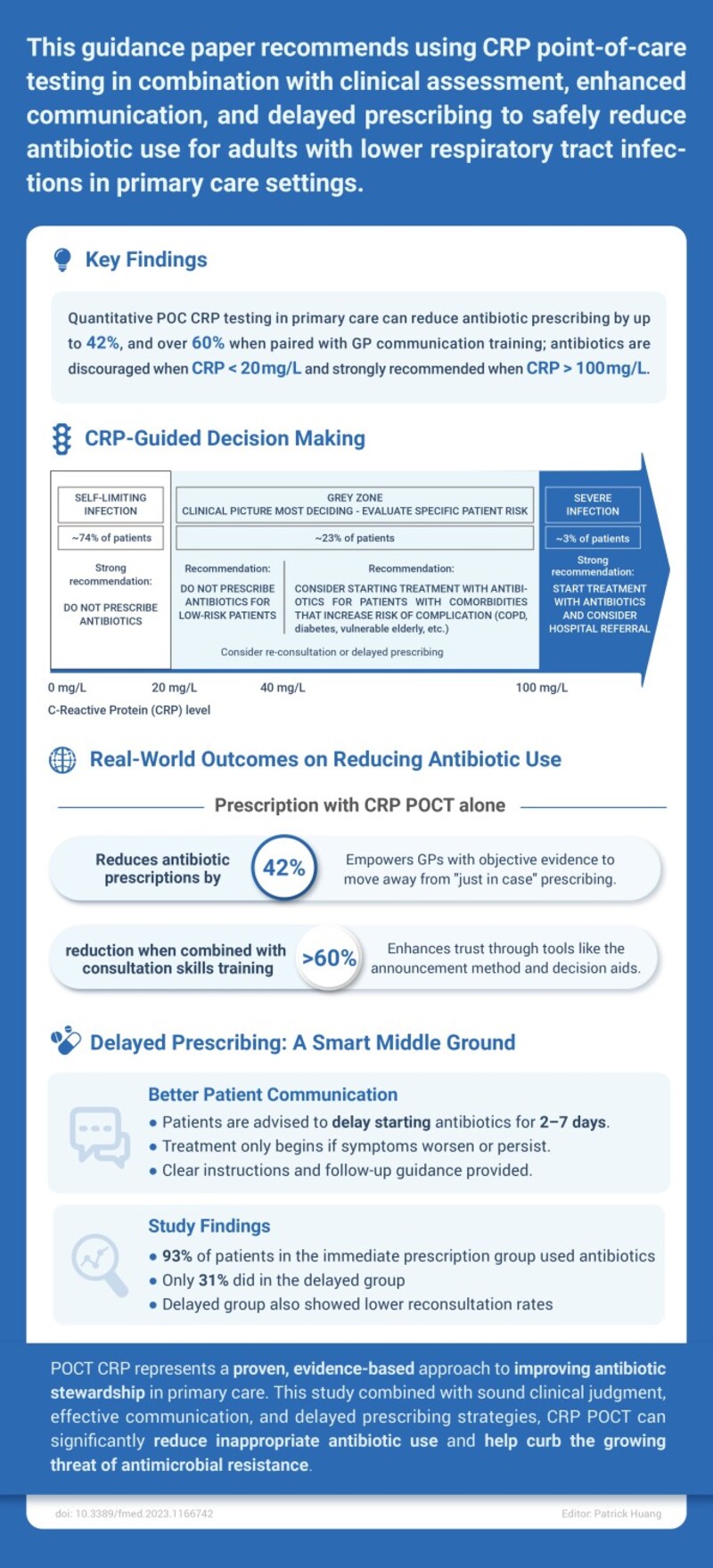
Clinical guidance increasingly recommends the use of C-reactive protein (CRP) point-of-care testing in combination with clinical assessment, enhanced patient communication, and delayed prescribing strategies to reduce unnecessary antibiotic use in adults with lower respiratory tract infections in primary care.
Key Evidence Supporting CRP POCT
Quantitative CRP testing in primary care has been shown to reduce antibiotic prescribing by up to 42%, with reductions exceeding 60% when combined with general practitioner (GP) communication training. Antibiotics are generally discouraged when CRP levels are below 20 mg/L and strongly recommended when levels exceed 100 mg/L.
CRP-Guided Clinical Decision Framework
CRP levels help stratify patients into clinically meaningful risk categories:
-
Self-limiting infections (CRP < 20 mg/L): Antibiotics are not recommended.
-
Intermediate-risk patients (CRP 20–100 mg/L): Treatment decisions should consider comorbidities and patient vulnerability, with delayed prescribing as an option.
-
Severe infections (CRP > 100 mg/L): Antibiotic therapy is recommended, with consideration of hospital referral when appropriate.
Delayed Prescribing as a Balanced Strategy
Delayed prescribing offers a middle-ground approach that balances patient reassurance and antibiotic stewardship. Patients are advised to delay antibiotic initiation for 2–7 days and begin treatment only if symptoms persist or worsen. Studies show that while 93% of patients in immediate prescription groups used antibiotics, only 31% did so in delayed prescribing groups, with lower reconsultation rates observed.
Clinical Significance
CRP POCT represents a proven, evidence-based approach to improving antibiotic stewardship in primary care. When combined with sound clinical judgment, effective communication, and delayed prescribing strategies, CRP testing can substantially reduce inappropriate antibiotic use and help address the growing challenge of antimicrobial resistance.
Reference:
doi: 10.3389/fmed.2023.1166742
 The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc.
The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc. 50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others.
50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others. Single-dose Chemiluminescense Immunoassay Platform
Single-dose Chemiluminescense Immunoassay Platform Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously.
Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously. Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals.
Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals. Ready-to-use lyophilized RT-PCR Reagent;
Ready-to-use lyophilized RT-PCR Reagent; Wondfo PA-3600 IHC Staining System
Wondfo PA-3600 IHC Staining System The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds.
The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds. This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.
This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.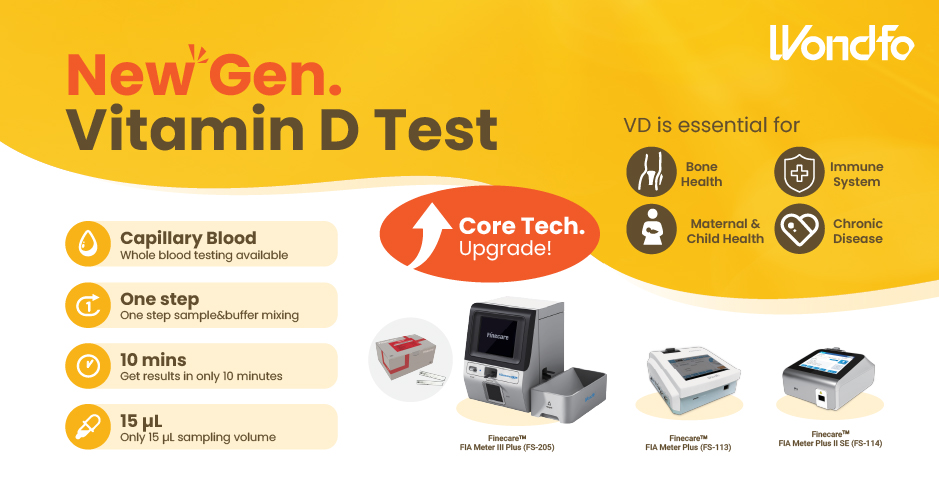 Finecare™ Vitamin D, from complexity to simplicity
Finecare™ Vitamin D, from complexity to simplicity Building A World Free from Antibitoic Overuse
Building A World Free from Antibitoic Overuse Advanced rapid diagnostic test with WHO prequalification for infectious disease
Advanced rapid diagnostic test with WHO prequalification for infectious disease The Future Intelligent Medical Assistant to Healthcare
The Future Intelligent Medical Assistant to Healthcare Fight against the pandemic through continuous innovation
Fight against the pandemic through continuous innovation