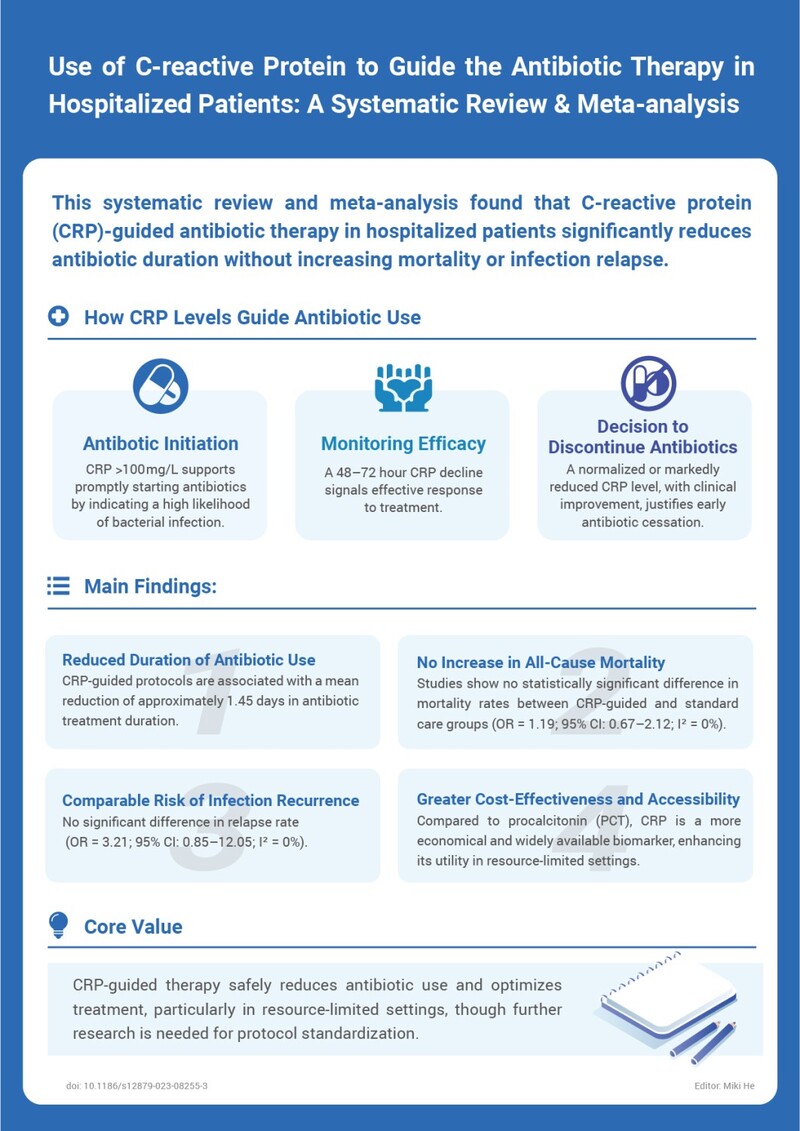
C-reactive protein (CRP) is a widely used inflammatory biomarker that has gained increasing attention for its role in guiding antibiotic therapy in hospitalized patients. A recent systematic review and meta-analysis evaluated the clinical impact of CRP-guided antibiotic strategies and demonstrated that CRP-based decision-making can safely reduce antibiotic exposure without compromising patient outcomes.
Role of CRP in Antibiotic Decision-Making
CRP levels provide valuable information throughout the course of infection management. Elevated CRP concentrations support the early identification of bacterial infections, while dynamic changes in CRP levels help clinicians assess treatment response and guide decisions on antibiotic discontinuation.
Key clinical applications of CRP include:
-
Antibiotic initiation: CRP levels above 100 mg/L indicate a high likelihood of bacterial infection and support timely initiation of antibiotic therapy.
-
Monitoring treatment efficacy: A decline in CRP levels within 48–72 hours suggests an effective therapeutic response.
-
Decision to discontinue antibiotics: Normalization or a marked reduction in CRP levels, together with clinical improvement, supports early cessation of antibiotic treatment.
Main Findings from the Meta-analysis
The analysis showed that CRP-guided antibiotic protocols are associated with a mean reduction of approximately 1.45 days in antibiotic treatment duration compared with standard care. Importantly, this reduction was achieved without an increase in adverse outcomes.
Key outcomes included:
-
No increase in all-cause mortality: No statistically significant difference was observed between CRP-guided and standard treatment groups.
-
Comparable risk of infection recurrence: Relapse rates were similar across groups, indicating that shorter antibiotic courses did not compromise infection control.
-
Improved cost-effectiveness: Compared with procalcitonin (PCT), CRP is more economical and widely available, making it particularly suitable for resource-limited settings.
Clinical Implications
CRP-guided antibiotic therapy represents a safe and effective strategy to optimize antibiotic use in hospitalized patients. While further research is needed to standardize protocols across clinical settings, current evidence supports the integration of CRP into antibiotic stewardship programs.
Reference:
doi: 10.1186/s12879-023-08255-3
 The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc.
The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc. 50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others.
50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others. Single-dose Chemiluminescense Immunoassay Platform
Single-dose Chemiluminescense Immunoassay Platform Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously.
Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously. Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals.
Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals. Ready-to-use lyophilized RT-PCR Reagent;
Ready-to-use lyophilized RT-PCR Reagent; Wondfo PA-3600 IHC Staining System
Wondfo PA-3600 IHC Staining System The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds.
The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds. This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.
This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.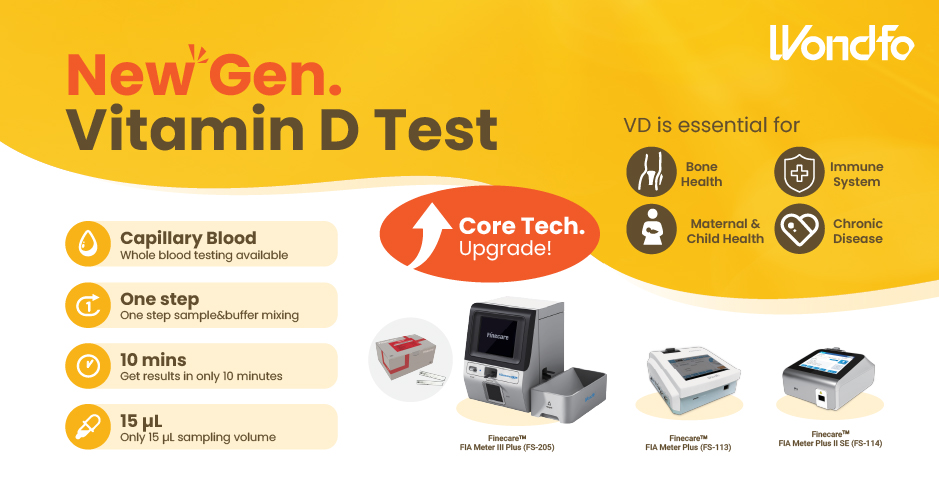 Finecare™ Vitamin D, from complexity to simplicity
Finecare™ Vitamin D, from complexity to simplicity Building A World Free from Antibitoic Overuse
Building A World Free from Antibitoic Overuse Advanced rapid diagnostic test with WHO prequalification for infectious disease
Advanced rapid diagnostic test with WHO prequalification for infectious disease The Future Intelligent Medical Assistant to Healthcare
The Future Intelligent Medical Assistant to Healthcare Fight against the pandemic through continuous innovation
Fight against the pandemic through continuous innovation