1. Introduction
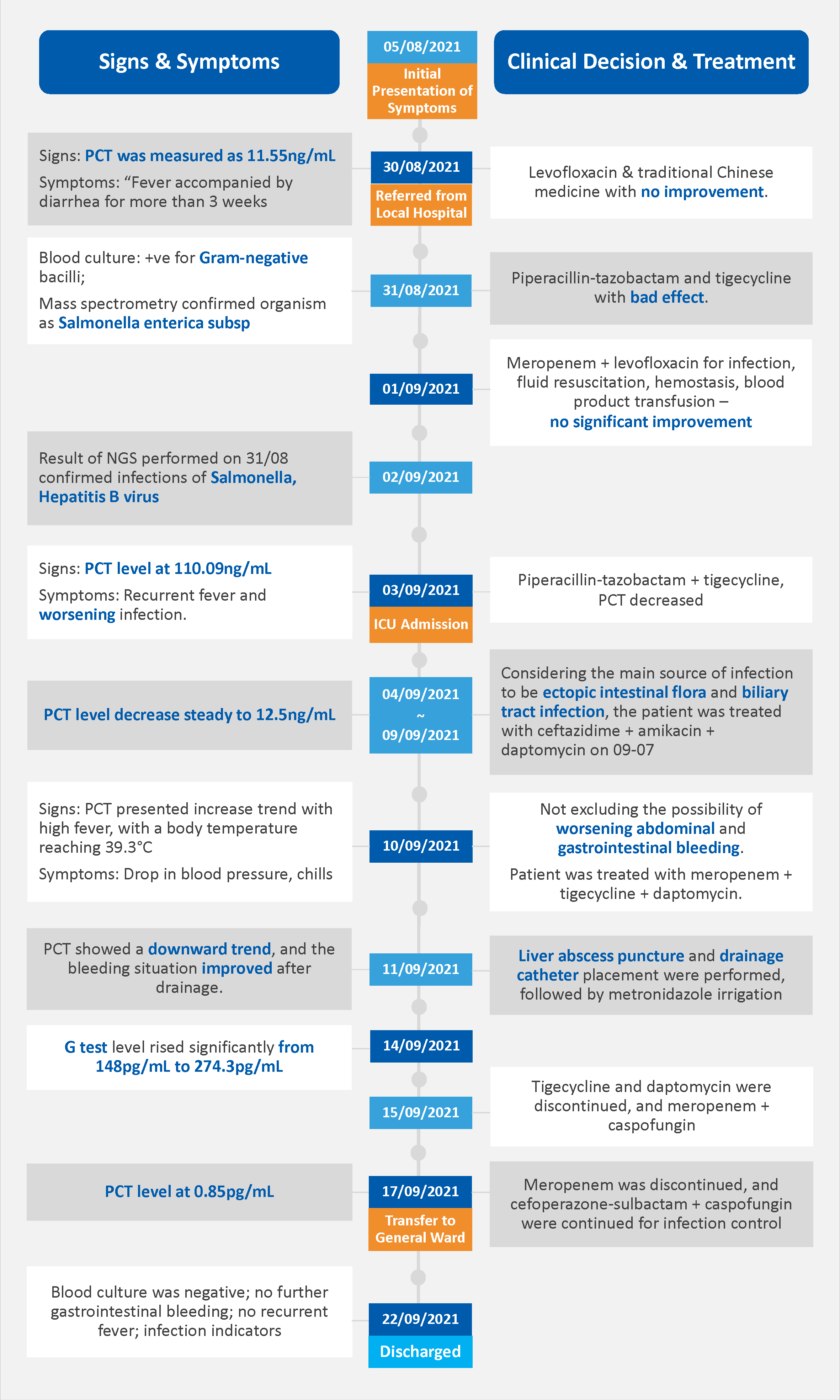
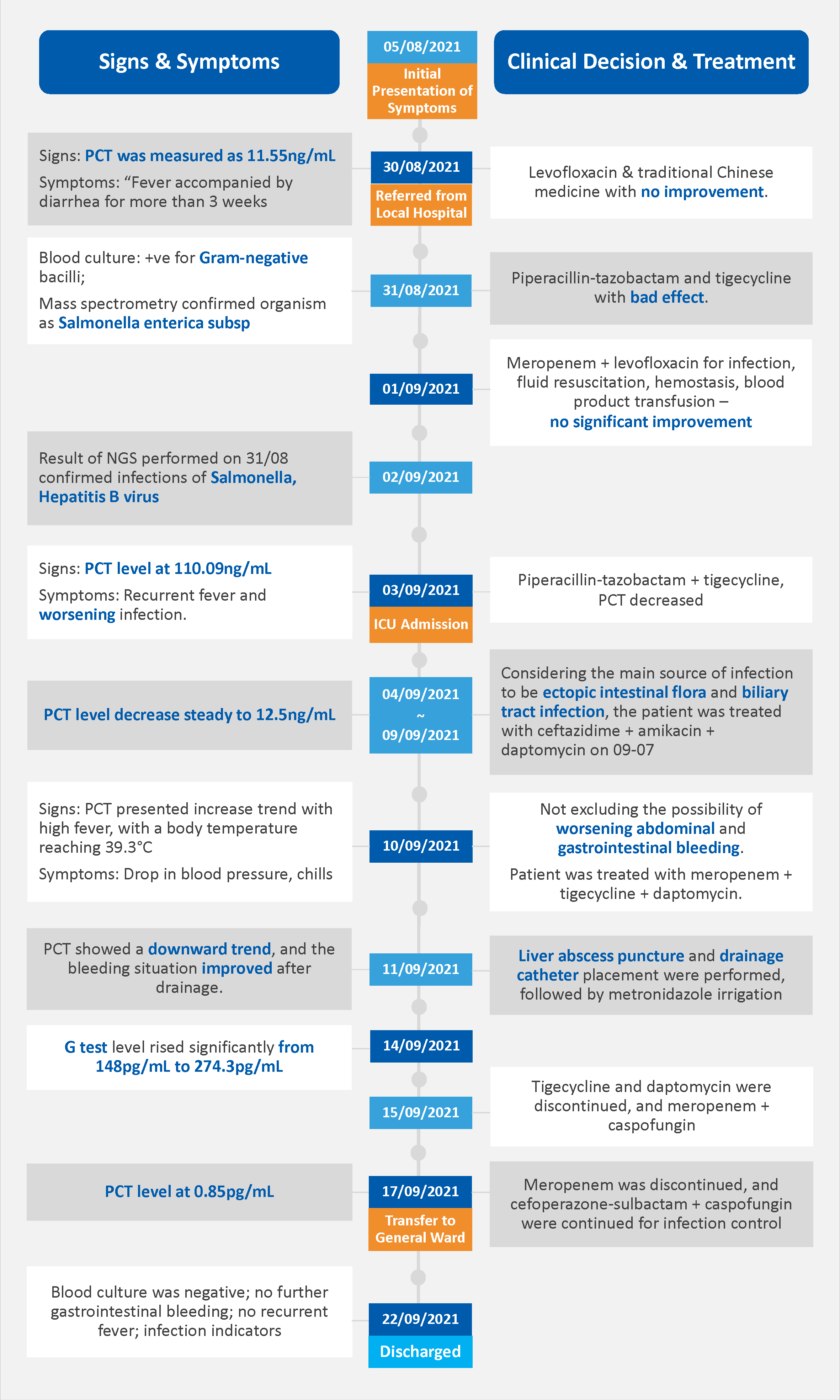
A 41-year-old male was admitted due to “fever accompanied by diarrhea for more than three weeks and discovery of a liver space-occupying lesion for five days.” After sweating and entering an air-conditioned room on August 5, 2021, he had chills and fever up to 39°C. From August 9, there were repeated chills and high fever up to 40°C, along with poor appetite, abdominal pain, and diarrhea. Treated with levofloxacin and traditional Chinese medicine with no improvement. The patient's clinical course and associated laboratory findings during hospitalization are detailed in the table below.
2. PCT Measurements and Clinical Course
2.1 Initial PCT Elevation and Infection Diagnosis
Upon admission, the patient’s procalcitonin (PCT) level was measured at 11.55 ng/mL, indicating a probable systemic bacterial infection. This elevation was consistent with the patient’s clinical presentation, which included persistent fever, diarrhea, and abdominal pain, as well as elevated inflammatory markers. Diagnostic imaging, including ultrasound and abdominal MRI, revealed a large mass in the right lobe of the liver, suggestive of hemorrhage and infection. Blood cultures were positive for Gram-negative bacilli, identified as Salmonella enterica through mass spectrometry, supporting the clinical suspicion of a severe bacterial infection.
2.2 PCT Fluctuations and Antibiotic Adjustments
Despite initial empirical antibiotic therapy with piperacillin-tazobactam and tigecycline, the patient’s condition did not improve, necessitating a reassessment of the antibiotic regimen. Subsequently, the treatment was modified to include meropenem and levofloxacin, in addition to supportive measures such as fluid resuscitation and blood product transfusions. However, the patient’s PCT levels surged to 110.09 ng/mL on September 3rd, concurrent with recurrent fevers and clinical signs of worsening infection. The source of infection was suspected to be secondary to translocated intestinal flora and biliary tract involvement. The antibiotic therapy was then adjusted to incorporate ceftazidime, amikacin, and daptomycin. On September 10th, the patient experienced a high fever, hypotension, chills, and abdominal bleeding, leading to the puncture and drainage of a liver abscess. Post-drainage, the PCT levels began to decrease, and the patient’s clinical status improved. By September 15th, tigecycline and daptomycin were discontinued, and meropenem was switched to caspofungin. The PCT levels subsequently normalized to 0.85 pg/mL, and the patient was discharged on September 22nd, free from fever and with no evidence of active infection.
3. The Role of PCT in Monitoring Antibiotic Treatments
3.1 Overview of PCT as a Biomarker
Procalcitonin (PCT) is a valuable biomarker for the diagnosis and differentiation of bacterial infections from viral infections, particularly in sepsis [1]. It has good discriminatory properties for differentiating bacterial and viral inflammations due to its synthesis being triggered by bacterial toxins and inhibited during viral infections [1]. PCT levels rise rapidly in response to bacterial infections, providing timely and reliable results for diagnosis [1]. PCT levels correlate with the severity of bacterial infections and can serve as a prognostic marker in sepsis management [1]. PCT is one of the most studied biomarkers in sepsis care and is increasingly being used in clinical practice, though further research is needed to optimize its use [1].
3.2 PCT-guided Antibiotic Management
PCT is effective in guiding antibiotic therapy by helping clinicians decide when to initiate or discontinue antibiotics [2]. PCT levels can guide de-escalation of antibiotics in critically ill patients with sepsis, potentially improving outcomes and reducing ICU stay [2]. Despite its benefits, PCT-guided antibiotic management may not always improve clinical outcomes and requires careful interpretation [2]. Several studies have demonstrated that PCT-guided antibiotic therapy can lead to a significant reduction in the length of antibiotic treatment and is associated with a significantly lower 28-day mortality [2]. However, there is a higher risk of recurrent infection [2].
In the context of antibiotic escalation, [3] found that using PCT to guide antibiotic escalation when pathogen evidence is unavailable could be associated with a shorter length of ICU stay for ICU patients with suspected bacterial infection. This suggests that PCT can be a useful tool for intensifying antibiotic therapy when faced with uncertain diagnoses [3].
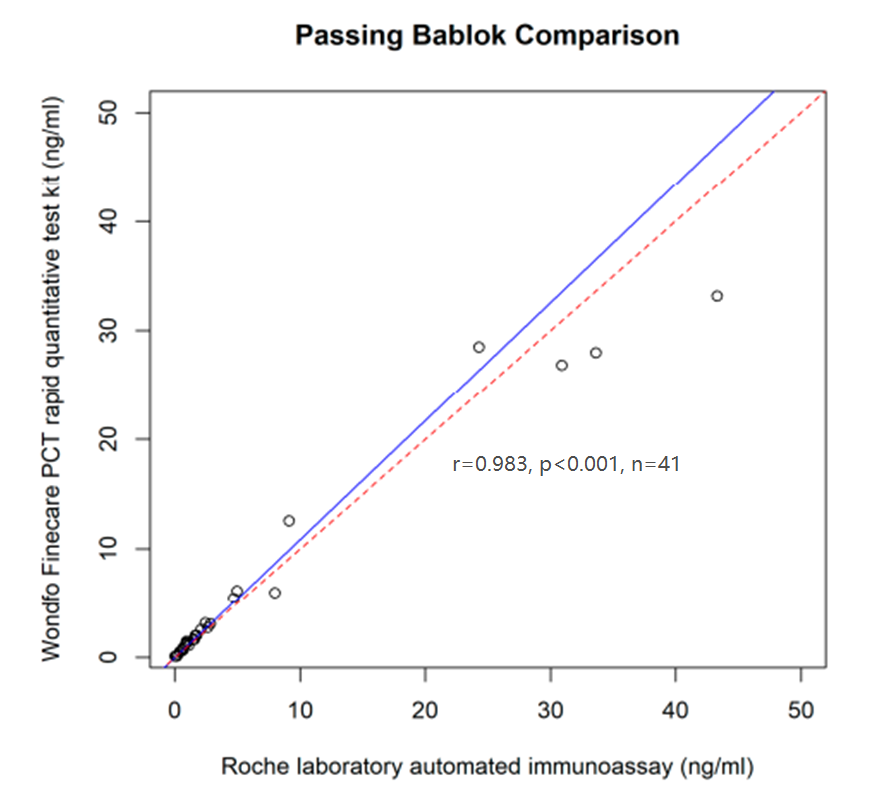
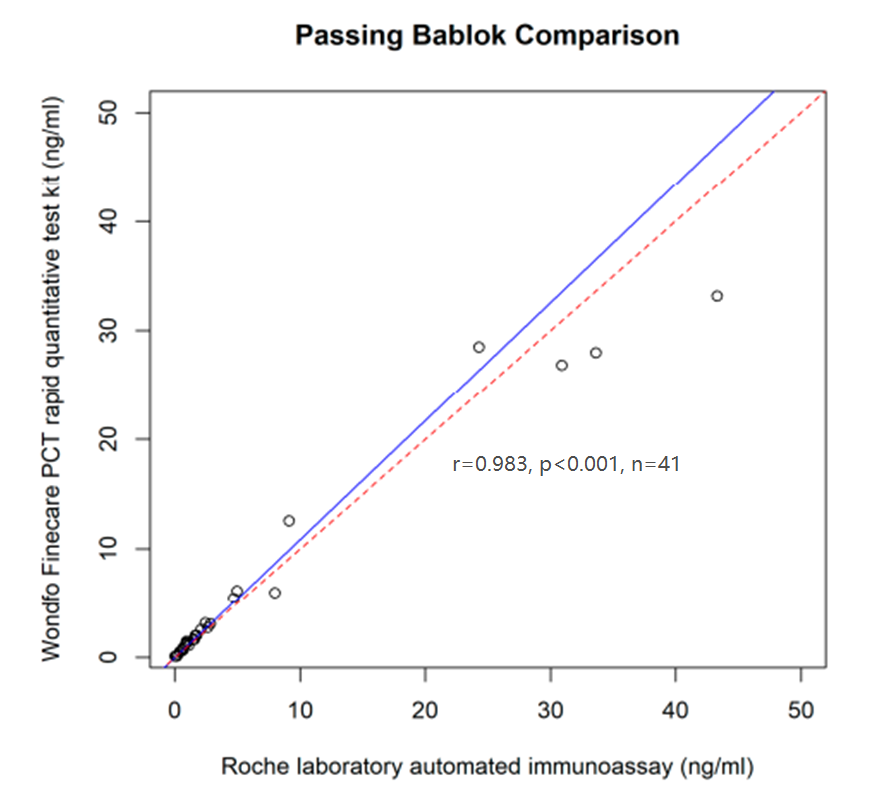
Notably, point-of-care (POC) PCT testing, specifically the Wondfo Finecare™ system, has been evaluated in an academic study [4], demonstrating comparable performance to reference laboratory immunoassays. The Wondfo Finecare™ POC test provides rapid and accurate results within minutes, facilitating prompt decision-making and antibiotic stewardship [4]. Another collaborative study reveals that Wondfo Finecare™ system PCT has 0.98 correlation comparing with Roche Elecsys system, and 5% CV for cutoff 0.5 ng/mL,demonstrating the excellent performance of Finecare system [4].


4. Conclusion
In conclusion, the use of PCT as a biomarker for antibiotic stewardship in sepsis has been shown to improve patient outcomes and reduce unnecessary antibiotic use. However, the optimal implementation of PCT in clinical practice requires careful consideration of individual patient factors and clinical context. Further research is needed to better understand how to integrate PCT into routine clinical care to maximize its benefits.
References:
1. Gregoriano, C., Heilmann, E., Molitor, A., & Schuetz, P. (2020). Role of procalcitonin use in the management of sepsis. Journal of Thoracic Disease, 12(Suppl 1), S5-S15. https://doi.org/10.21037/jtd.2019.11.63
2. Papp, M., Kiss, N., Baka, M., Trásy, D., Zubek, L., Fehérvári, P., Harnos, A., Turan, C., Hegyi, P., & Molnár, Z. (2023). Procalcitonin-guided antibiotic therapy may shorten length of treatment and may improve survival—a systematic review and meta-analysis. Critical Care, 27(394). https://doi.org/10.1186/s13054-023-04677-2
3. Wang, X., Long, Y., Su, L., Zhang, Q., Shan, G., & He, H. (2022). Using procalcitonin to guide antibiotic escalation in patients with suspected bacterial infection: A new application of procalcitonin in the intensive care unit. Frontiers in Cellular and Infection Microbiology, 12(844134). https://doi.org/10.3389/fcimb.2022.844134
4. Mazlan, M.Z., Wan Azman, W.N., Yaacob, N.M., Koon, T.S., & Yahya, N.K. (2024). Analytical Evaluation of Point-of-Care Finecare™ Procalcitonin Rapid Quantitative Test in Sepsis Population as Compared with Elecsys® BRAHMS Procalcitonin Immunoassay. Diagnostics, 14(1080). https://doi.org/10.3390/diagnostics14111080
 The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc.
The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc. 50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others.
50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others. Single-dose Chemiluminescense Immunoassay Platform
Single-dose Chemiluminescense Immunoassay Platform Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously.
Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously. Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals.
Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals. Ready-to-use lyophilized RT-PCR Reagent;
Ready-to-use lyophilized RT-PCR Reagent; Wondfo PA-3600 IHC Staining System
Wondfo PA-3600 IHC Staining System The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds.
The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds. This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.
This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.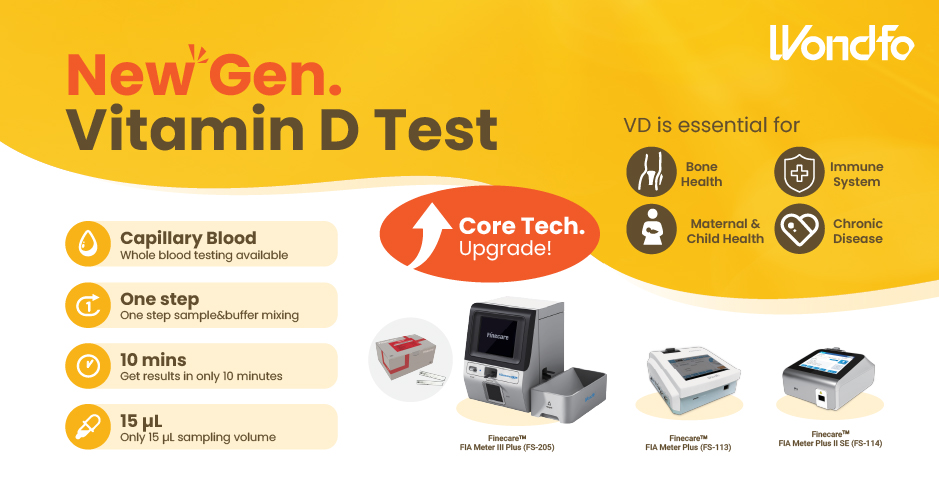 Finecare™ Vitamin D, from complexity to simplicity
Finecare™ Vitamin D, from complexity to simplicity Building A World Free from Antibitoic Overuse
Building A World Free from Antibitoic Overuse Advanced rapid diagnostic test with WHO prequalification for infectious disease
Advanced rapid diagnostic test with WHO prequalification for infectious disease The Future Intelligent Medical Assistant to Healthcare
The Future Intelligent Medical Assistant to Healthcare Fight against the pandemic through continuous innovation
Fight against the pandemic through continuous innovation