In 1910, the first antimicrobial agent, salvarsan, was deployed followed by a huge batch of antimicrobials emerged in just over 100 years, which have drastically changed the world. As killers of microorganisms, antimicrobials treat and prevent bacterial infection and subsequent deaths, greatly expanding people’s lifespan. However, underneath the benefits brought by antibiotics lurks the undiscovered risk of antimicrobial misuse.
Mismatched target and killer lead to no good outcome
Antimicrobials, including antibiotics, antivirals, antifungals and antiparasitics, work by inhibiting the activity of specific substance. For example, oseltamivir phosphate is an oral antiviral drug by inhibiting the activity of the viral neuraminidase enzyme found on the surface of the virus and preventing dubbing from the hose cell, replication and infectivity. But oseltamivir only kills flu viruses and does not work for bacterial infections. Taking improper pills not only fails to alleviate the symptoms but also lead to worse outcome with delayed treatment.
When suspicious symptoms for infection occur, a primary differentiation can greatly avoid misuse of antimicrobials. As flu season approaches against the backdrop of Covid pandemic, we are confronted with an ever-more complicated coalition of multiple viruses sharing similar symptoms like coughing, sneezing and fever. Children, the elderly and the pregnant are especially susceptible to infection and sometimes have difficulty in going to hospital. To facilitate early diagnosis and differentiation of viral infection, more and more at-home rapid test kits are available to detect
COVID-19 infection,
Flu A/B infection and
Strep A infection. These self-test kits improve access to diagnosis and safeguard people’s lives and happiness.
Risks for antimicrobial resistance in medication
Antibiotics can be categorized into broad-spectrum and narrow-spectrum antibiotics. Broad-spectrum antibiotics can kill most bacteria, while narrow-spectrum antibiotics target at a specific kind of bacteria. Broad-spectrum antibiotics target a wide range of microorganism and reduce the total richness and maturity of the microbiota. Narrow-spectrum antibiotics are more preferred as they kill only those unwanted species causing diseases and leave most of the beneficial bacteria unaffected. However, one disadvantage of narrow-spectrum antibiotics is that the identity of the bacterium needs to be known in advance. By using antibiotics when they are not needed can lead to antibiotic-resistant bacteria that are extremely hard to treat, which is also known as superbugs.
When a certain antimicrobial pill kills its targeted micro-organisms, part of them that survive can adapt to the antimicrobial drug and develop resistance towards it. As such germs approach various kinds of antimicrobials, they gradually develop stronger resistance, and then drugs become ineffective to them. Such resistance can be transmitted through genes, creating even stronger germs.
The generation of pandrug-resistant bacteria—superbugs—is accelerated by antimicrobial misusing, such as
• taking wide-spectrum antibiotics
• taking improper antimicrobials without determining pathogen
• taking antimicrobials as preventive measures
• taking pills without following prescription
Usually laboratory testing is taken to aid in diagnosis at the admission into hospital. Common testing menu include CBC, ESR, CRP and PCT. Microbiological culture is usually regarded as the standard basis for diagnosis, but it takes one to five days to get a result. Routine blood tests, antigen test and PCR tests are suggested for primary diagnosis before the pending culture result is released. In recent years, PCT has been widely recognized for its specificity in differentiating between bacterial and non-bacterial inflammation and is usually taken over consecutive days to help healthcare providers assess the response to antibiotic therapy in case of excessive exposure to antimicrobials. With Finecare FIA Meters,
CRP, SAA, PCT, IL-6 and CRP/PCT combo tests have been marked with CE. With portable instrument and room-temperature stable reagents, rapid results are released in 3-15 minutes. Rapid CRP and SAA tests with fingertip blood are available now for faster and easier testing in various scenarios such as pharmacy and clinic.
As World Antimicrobial Awareness Week is celebrated from 18 to 24 November every year, more awareness is called for preventing antimicrobial resistance. Please do not let the cure today become a killer tomorrow. Make the antimicrobial work when it is supposed to.
 The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc.
The first developed technology platform with various application scenarios, including infectious disease, fertility, DOA, etc. 50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others.
50+ kinds of reagents and five high-performance devices, focusing on detecting cardiovascular disease, inflammation, kidney injury, sex hormones, thyroid function, diabetes, tumor, and others. Single-dose Chemiluminescense Immunoassay Platform
Single-dose Chemiluminescense Immunoassay Platform Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously.
Wondfo optical blood coagulation analyzer is the first one in the world that can test PT, APTT, TT, FIB, and ACT simultaneously. Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals.
Our Blood Gas Analyzer BGA-102 can produce the result in 30s. Its advantages of portability, easy operation, durability, and high performance make it ideal for clinics, laboratories, and hospitals. Ready-to-use lyophilized RT-PCR Reagent;
Ready-to-use lyophilized RT-PCR Reagent; Wondfo PA-3600 IHC Staining System
Wondfo PA-3600 IHC Staining System The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds.
The Wondfo Truth-H80E HPLC Hemoglobin Analyzer is a high-performance diagnostic device designed for rapid and precise measurement of glycosylated hemoglobin (HbA1c)—the gold standard for diabetes diagnosis.It support the standard mode and variant mode and provide the result within 60-90seconds. This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.
This year, the summit will place a special focus on collaboration across different fields to explore the application of POCT and optimize clinical pathways. In the meantime, drive innovation by adoption of new technologies and biomarkers.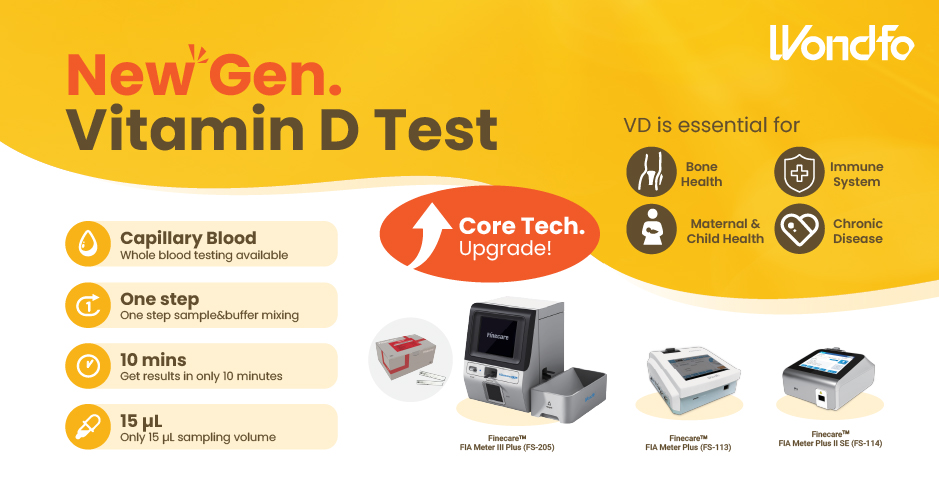 Finecare™ Vitamin D, from complexity to simplicity
Finecare™ Vitamin D, from complexity to simplicity Building A World Free from Antibitoic Overuse
Building A World Free from Antibitoic Overuse Advanced rapid diagnostic test with WHO prequalification for infectious disease
Advanced rapid diagnostic test with WHO prequalification for infectious disease The Future Intelligent Medical Assistant to Healthcare
The Future Intelligent Medical Assistant to Healthcare Fight against the pandemic through continuous innovation
Fight against the pandemic through continuous innovation